PTSD And Young Veteran Suicide
As the rate of veteran suicide rate increases, awareness and action are slow to follow.
 Post-Traumatic Stress Disorder affects scores of Americans, a hefty number of them veterans. The severity of the disorder can range from flashbacks, panic attacks triggered by sounds, tactile sensations, or even certain words to insomnia and self-destructive behaviors. PTSD, as it is commonly known, is harsh on the life of a homebound veteran, and often requires therapy and/or medication to assist in rehabilitation—and NOW.
Post-Traumatic Stress Disorder affects scores of Americans, a hefty number of them veterans. The severity of the disorder can range from flashbacks, panic attacks triggered by sounds, tactile sensations, or even certain words to insomnia and self-destructive behaviors. PTSD, as it is commonly known, is harsh on the life of a homebound veteran, and often requires therapy and/or medication to assist in rehabilitation—and NOW.
Holding a job can be difficult, and this affects income and ability to provide oneself with housing and proper accommodations. This is why many people with PTSD, especially veterans, are at risk for homelessness. Among mental illnesses plaguing the homeless, PTSD is one of the most common. When left improperly treated, or not treated , self-destructive behavior caused by PTSD can cause suicide.
At least 22 veterans are lost to suicide daily according to 2014 studies, especially young males under 30. Young veterans are twice as likely to have their lives ended by suicide than civilian men in the same age range.
What is PTSD?
Mental illnesses manifest physically and through behavioral symptoms. To properly treat Post-Traumatic Stress Disorder, it must be understood by professionals. It usually comes from a traumatic event, cluster of events, or prolonged trauma that severely affects natural stress responses. It is often a lifelong problem and can affect a veteran’s life from the moment they return home. Symptoms include:
- Flashbacks
- Insomnia and nightmares relating to the event
- Agitation and hostility
- Hypervigilance
- Unwanted thoughts
- Some may even experience hallucinations and hear voices
When veterans are exposed to high-stress situations or witness a devastating event (especially if they are already predisposed to anxiety or stress responses) they become at risk for developing PTSD. In flashbacks, they may physically or emotionally relive the event, or disassociate and believe they are back at the scene. In severe cases, patients may hear intrusive voices that promote self-destructive and out of character behavior.
How does it affect the brain?
When stressed, our brain signals our body to respond. Pupils dilate, muscles become stiff, and we think faster while becoming more vigilant. For most people, this is a temporary state. But for people with PTSD, the brain can almost constantly be in a state of “fight or flight” thanks to the release of the stress hormone cortisol. Chronic stress can even damage the physical brain structure.
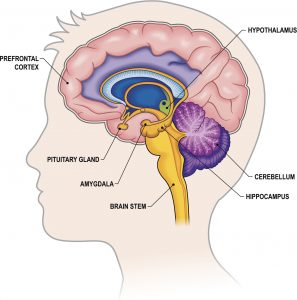
The amygdala is a part of the brain that contributes to the control of a fight or flight response. Normally, parts of our brain that contribute to higher, more logical ways of thinking can calm us down. For example, thunder might frighten some with its sudden noise, but logic may calm us by remembering that thunder is just a noise that does not pose direct harm. In someone with impaired access to that thinking with an overactive amygdala and PTSD, the noise may remind them of the sound of combat and trigger a flashback.
PTSD also affects the memory. The hippocampus is another part of the brain involved in memory. It can help provide some logical context to the current stressful circumstances and calm the stress response. Affected by the disorder, it may not be able to perform those duties. In younger veterans, the brain may still be developing, making this impact even more powerful and dealing a harsh blow to readjusting to civilian life. This is one reason the young veteran suicide rate is so high.
Veterans’ Health
Returning troops suffer from PTSD at a rate of 15%, and have to wait to see specialists. The VHA currently has hundreds of thousands of claims left unprocessed as a backlog, making access to much needed treatment incredibly difficult. Private practitioners, if veterans can reach them, may not be able to properly treat the unique experiences of veterans, and inpatient units may not prevent an attempted suicide due to lack of quality care, poor staffing and leadership. Without proper coordination, attention and compassion, veterans in inpatient units can die a preventable death. Failing to prevent suicide is something providers must be held accountable, especially for veterans returning from duty.
Action can prevent suicide. Enrollment in the VHA has proven to help, as veterans have access to support and care, and a community. But funding and direction towards these resources is still lacking. Some veterans are simply brought home and left without direction, or on a long waiting list. Action can save lives, and our veterans deserve the treatment they need to make up for what they’ve lost in the line of duty. Some veterans have even died by suicide while waiting to receive mental health treatment. The lines are simply too long, and the stigma surrounding mental illness remains a problem. Work must be done to dismiss the myths that PTSD is a form of weakness and fragility-it is a wound that must be cared for. Many veterans are falling through the cracks of the mental health system, resulting in suicides.
VA’s have attempted to help the overload problem with access to crisis centers and community service boards, but these treatments are inadequate to address a long-term problem, and even they have a backlog. They are understaffed and underfunded, and as a result, veterans suffer and die.
Skip Simpson says “there is no urgency to fix the mental health problems for our vets. The delays our vets experience exacerbate PTSD—stress does that. Trying to navigate a system while suffering from a mental illness is tough. Lots of ‘happy talk’ about the vet’s welfare is disgusting. One can imagine what the young man or woman– fighting to live– thinks when he or she watches the confusion in Washington D.C. It seems the politicians think only of themselves and not those they are sworn to serve.”
We can help
If you or someone you know has lost a loved one to veteran suicide, we’re here for you. Suicide is preventable with the right care, and failing to provide it can cause tragedy. At the Law Offices of Skip Simpson, we offer a free case evaluation to survivors suffering and looking for answers for those held accountable. Help should be given, not chased down with no results. Our veterans have protected us, and now it is the system’s responsibility to give back. How many times have we heard those words? When the vet hears them with no action, it is just another reason to give up. Contact us today to take the first step towards justice.