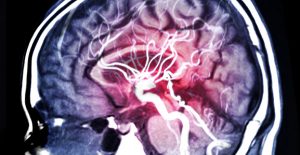
Brain scans may ID suicide risks linked to depression
 Even though the majority of people with depression don’t die by suicide, statistics show that roughly 30 percent who are unaffected by multiple antidepressant drugs or therapy make at least one attempt in their lifetime.
Even though the majority of people with depression don’t die by suicide, statistics show that roughly 30 percent who are unaffected by multiple antidepressant drugs or therapy make at least one attempt in their lifetime.
A common misconception about depression is that it must be treated as a single condition. However, it often involves multiple ailments that can heighten the risk of suicide, according to Science Mag. Researchers are currently trying to identify several depression subtypes by comparing the neural circuits that light up during certain tasks with actual depression symptoms. These efforts are part of a larger initiative to delve deeper into brain biology and mental health.
Identifying subtypes of depression that are most often linked to suicide
While the ultimate goal is to identify suicide risks through biological means, researchers hope to develop effective strategies for care that extend far beyond conventional psychiatry. This effort includes Research on Anxiety and Depression-Anhedonia Treatment (RAD-AT), which enrolls volunteers with certain subtypes of depression that put them at a heightened risk of suicide.
The study — which is led by Leanne Williams, a Stanford clinical neuroscientist — pioneers a method of treatment based on brain circuitry. In addition, the study hopes to link symptoms of depression to brain biology in order to help those who have had no previous success with treatment.
For more than 20 years, Williams has studied how depression manifests in the brain and has worked to collect thousands of brain scans from people with depression. After losing a patient early in her career, and recently, a loved one, she has dedicated herself to preventing death by suicide in people with depression.
After extensive research, Williams has identified at least six subtypes of depression, each of which is generated by unusual activity in the brain that effects certain sets of circuits responsible for regulating mood and cognition. Three key subtypes were found to be linked to suicide risks. These include:
- A subtype that affects a circuit called the default mode network, which creates aimless mental chatter and negative thoughts while the brain is in neutral.
- Another subtype, also called anhedonia, affects the reward networks — causing those affected by it to feel little or no pleasure.
- A third subtype associated with attention, planning, and impulse (called cognitive control) often doesn’t respond adequately to depression treatment.
The link between brain biology and suicide has been studied since the early 1980s, particularly by neuroscientist John Mann of Columbia University. After examining the brains donated by families of those who died by suicide, he found that levels of serotonin were significantly lower than depressed people who died in other ways.
What other research has concluded
Mann recently joined Maria Oquendo, a psychiatrist at the University of Pennsylvania, to further study the link between low serotonin levels and suicide. In a 2016 study, Mann and Oquendo compiled data from positron emission tomography (PET) imaging, which tracks serotonin levels in the brain by using radioactive labels.
The study, which included 100 participants who were depressed or suicidal, found a significant biological difference between people with low-serotonin levels and those who experience circumstantial suicidal thoughts.
Another study, which was led by neuroscientist Irina Esterlis at Yale University focused exclusively on the link between post-traumatic stress disorder (PTSD) and suicide. The study also used PET imaging, which found that people with PTSD who experienced suicidal thoughts were deficient in the signaling molecule glutamate. Esterlis’s finding also explores the possibility of treatment with a drug called ketamine, which may help with glutamate deficiency.
Skeptics believe that there is no one way to identify depression subtypes. Some research suggests indicators of depression subtypes may be based on distinct symptoms, response to treatment, genetics, hormones, and gut bacteria.
What we do know is, suicidal thoughts often occur in people who, otherwise, live seemingly satisfying lives. For this reason, conventional psychiatry may not be effective at mitigating the risk. You can’t simply ask a person suffering from depression why they feel depressed. The biological markers in the brain simply can’t be expressed in words.
We hope that the findings from this research lead to effective measures of identifying biologically related suicide risks and administering effective treatment.
If you have lost a loved one due to death by suicide, you may be looking for answers and closure. An experienced Texas suicide lawyer at the Law Offices of Skip Simpson can help you through these difficult times. We’re dedicated to helping families seek justice. Contact us online today to schedule a free case evaluation with our legal team.




